Remote Patient Monitoring (RPM) System
A Remote Patient Monitoring (RPM) System is a patient monitoring system that can solve a remote patient monitoring task (to monitor a patient at a distance, usually at home).
- Context:
- It can (typically) connect to remote and/or wearable medical devices
- It can it can connect to a Body Sensor Network (BSN).
- It can range from being a Single-Sensor Monitoring to being a Multi-Sensor Monitoring System.
- It can range from being a Online Health Monitoring System, to being a Smartphone-based Health Monitoring System, to being a Wearable Health Monitoring System.
- …
- Example(s):
- Counter-Example(s):
- See: mHealth, Telemedicine, Digital Medicine, Telehealth, Remote Sensing, Biosensor, Decentralized Clinical Trial.
References
2022
- https://news.crunchbase.com/health-wellness-biotech/remote-patient-monitoring-funding-general-prognostics/
- QUOTE: ... The goal of RPM devices was meant to help doctors track their patients between appointments, and develop a better snapshot of how patients fared in their everyday lives outside of the clinic. ... This was especially crucial for patients with chronic conditions with poor disease management, and would allow the doctor to intervene before an upcoming appointment. ...
2021a
- (Wikipedia, 2021) ⇒ https://en.wikipedia.org/wiki/Remote_patient_monitoring Retrieved:2021-10-3.
- Remote patient monitoring (RPM) is a technology to enable monitoring of patients outside of conventional clinical settings, such as in the home or in a remote area, which may increase access to care and decrease healthcare delivery costs. RPM involves the constant remote care of patients by their physicians, often to track physical symptoms, chronic conditions, or post-hospitalization rehab.[1]
Incorporating RPM in chronic-disease management may significantly improve an individual's quality of life, by allowing patients to maintain independence, prevent complications, and to minimize personal costs.[2] RPM facilitates these goals by delivering care through telecommunications. This form of patient monitoring can be particularly important when patients are managing complex self-care processes such as home hemodialysis. Key features of RPM, like remote monitoring and trend analysis of physiological parameters, enable early detection of deterioration; thereby reducing emergency department visits, hospitalizations, and the duration of hospital stays.[3] [4] [5] [6] While technologies are continually being developed to tackle this type of health care, physicians may utilize basic communication methods such as Zoom, Snapchat, or even landline phones. Pilot programs for Remote Patient Monitoring began in the 1970's when Kaiser Permanente created monitoring systems for rural communities in order to provide better healthcare to isolated regions. Literature related to Remote Patient Monitoring suggests that interventions based on health behavior models, care pathways, and personalized coaching lead to the best outcomes.[7] Research on the use of Remote Patient Monitoring technologies has helped determine that further development of telehealth ecosystems, in which physicians can give recommendations and means of care while also receiving transmitted health information, can lead to better patient outcomes and higher patient satisfaction. [8] Researchers also note that Remote Patient Monitoring will become more important as healthcare changes from a volume focus to a value focus. During the COVID-19 pandemic, Remote Patient Monitoring has been used extensively and allowed for more fields such as psychology or cardiology to use virtual care. By 2025, the Remote Patient Monitoring industry is expected to double, due to factors such as the COVID-19 pandemic and increased at-home care. Use of Remote Patient Monitoring has been proven to ultimately provide better patient compliance and improved physician management, while decreasing costs of care.
- Remote patient monitoring (RPM) is a technology to enable monitoring of patients outside of conventional clinical settings, such as in the home or in a remote area, which may increase access to care and decrease healthcare delivery costs. RPM involves the constant remote care of patients by their physicians, often to track physical symptoms, chronic conditions, or post-hospitalization rehab.[1]
- ↑ Wicklund E, ed. (4 May 2021). "How COVID-19 Affects the Telehealth, Remote Patient Monitoring Landscape". mHealthIntelligence. Retrieved 2021-08-19.
- ↑ Bayliss EA, Steiner JF, Fernald DH, Crane LA, Main DS (2003). [Bayliss EA, Steiner JF, Fernald DH, Crane LA, Main DS (2003). “Descriptions of barriers to self-care by persons with comorbid chronic diseases". Annals of Family Medicine. 1 (1): 15–21. doi:10.1370/afm.4. PMC 1466563. PMID 15043175. “Descriptions of barriers to self-care by persons with comorbid chronic diseases"]. Annals of Family Medicine. 1 (1): 15–21. doi:10.1370/afm.4. PMC 1466563. PMID 15043175.
- ↑ "Technologies for remote patient monitoring in older adults: Position paper" (PDF). Oakland, CA: Center for Technology and Aging. April 2010.
- ↑ O'Donoghue J, Herbert J (2012). “Data Management within mHealth Environments: Patient Sensors, Mobile Devices, and Databases". J. Data and Information Quality. 4: 1–20. doi:10.1145/2378016.2378021. S2CID 2318649.
- ↑ Coye MJ, Haselkorn A, DeMello S (2009). "Remote patient management: technology-enabled innovation and evolving business models for chronic disease care". Health Affairs. 28 (1): 126–35. doi:10.1377/hlthaff.28.1.126. PMID 19124862.
- ↑ Vavilis S, Petković M, Zannone N (2012). "Impact of ICT on home healthcare" (PDF). In ICT Critical Infrastructures and Society. Berlin, Heidelberg: Springer. pp. 111–122.
- ↑ Noah B, Keller MS, Mosadeghi S, Stein L, Johl S, Delshad S, et al. (January 2018). "Impact of remote patient monitoring on clinical outcomes: an updated meta-analysis of randomized controlled trials". NPJ Digital Medicine. 1 (1): 20172. doi:10.1038/s41746-017-0002-4. PMC 6550143. PMID 31304346.
- ↑ Riaz MS, Atreja A (December 2016). "Personalized Technologies in Chronic Gastrointestinal Disorders: Self-monitoring and Remote Sensor Technologies". Clinical Gastroenterology and Hepatology. 14 (12): 1697–1705.
2021b
- (Bayoumy et al., 2021) ⇒ Karim Bayoumy, Mohammed Gaber, Abdallah Elshafeey, Omar Mhaimeed, Elizabeth H. Dineen, Francoise A. Marvel, Seth S. Martin, Evan D. Muse, Mintu P. Turakhia, Khaldoun G. Tarakji, Mohamed B. Elshazly (2021). "Smart wearable devices in cardiovascular care: where we are and how to move forward". In: Nature Reviews Cardiology, 18.
- QUOTE: Technological innovations reach deeply into our daily lives and an emerging trend supports the use of commercial smart wearable devices to manage health. In the era of remote, decentralized and increasingly personalized patient care, catalysed by the COVID-19 pandemic, the cardiovascular community must familiarize itself with the wearable technologies on the market and their wide range of clinical applications
2021c
- (Pennic, 2021) ⇒ Jasmine Pennic (2021). "Swift Medical Launches AI Digital Wound App to Support Clinical Trials". In: HIT Consultant.
- QUOTE: Swift Medical's first product, Swift Skin and Wound, provides an AI-powered, digital wound platform that allows any patient or clinician to easily capture high-precision images of skin or wound conditions with any smartphone camera. Swift Skin and Wound autonomously determines clinical characteristics, tracks disease progression, enables remote communication, and securely shares patient data in real-time.
2018a
- (Noah, 2018) ⇒ Benjamin Noah, Michelle S. Keller, Sasan Mosadeghi, Libby Stein, Sunny Johl, Sean Delshad, Vartan C. Tashjian, Daniel Lew, James T. Kwan, Alma Jusufagic, and Brennan M. R. Spiegel (2018). "Impact of remote patient monitoring on clinical outcomes: an updated meta-analysis of randomized controlled trials". In: npj Digital Medicine. DOI:h10.1038/s41746-017-0002-4.
- QUOTE: The ability of wearable biosensors to passively capture and track continuous health data gives promise to the field of health informatics, which has recently become an area of interest for its potential to advance precision medicine [1]. The concept of leveraging technological innovations to enhance care delivery has many names in the healthcare lexicon. The terms digital health, mobile health, mHealth, wireless health, Health 2.0, eHealth, quantified self, self-tracking, telehealth, telemedicine, precision medicine, personalized medicine, and connected health are among those that are often used synonymously (Atallah et al., 2012). A 2005 systematic review uncovered over 50 unique and disparate definitions for the term e-health in the literature (Banaee et al. 2013). A similar 2007 study found 104 individual definitions for the term telemedicine (Dobkin and Dorsch, 2011). For the purpose of this study, we employ the term remote patient monitoring (RPM) and define it as the use of a non-invasive, wearable device that automatically transmits data to a web portal or mobile app for patient self-monitoring and or health provider assessment and clinical decision-making.
- ↑ (Andreu-Perez et al., 2015) ⇒ Javier Andreu-Perez, Daniel R. Leff, H. M. D. Ip, and Guang-Zhong Yang (2015)." From Wearable Sensors to Smart Implants--Toward Pervasive and Personalized Healthcare. In: IEEE Transactions on Biomedical Engineering (Volume: 62, Issue: 12). DOI: 10.1109/TBME.2015.2422751.
2018b
- (Yetisen et al., 2018) ⇒ Ali K. Yetisen, Juan Leonardo Martinez-Hurtado, Baris Unal, Ali Khademhosseini, and Haider Butt (2018). "Wearables in Medicine". In: Advanced Materials, 30(33), 1706910. DOI: 10.1002/adma.201706910
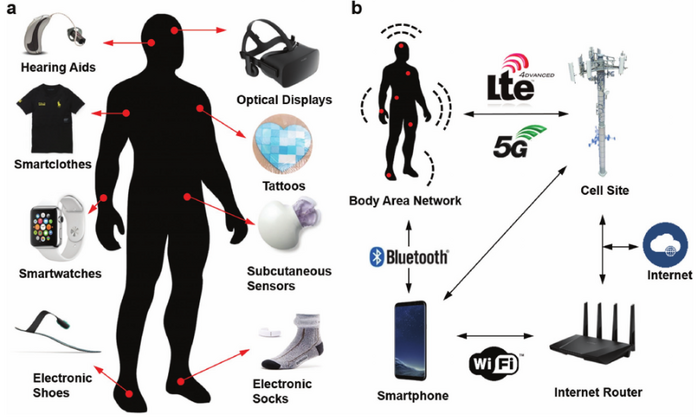
- QUOTE: In combination with value-based healthcare systems through telehealth, wearable devices can enable monitoring at risk patients, intervening diseases at an earlier stage, and reducing healthcare expenditures by means of prediction and prevention of disease. These wearable technologies include smartwatches, wristbands, hearing aids, electronic optical tattoos, head-mounted displays, subcutaneous sensors, electronic footwear, and electronic textiles (Figure 1a). They can be conformably placed on the epidermis, inserted through the skin or body orifices for measuring electrophysiological or biochemical signals, and delivering drugs. Such technologies when incorporated in garments, accessories, or epidermal surface to provide electronic alerts, sense physical and biochemical information, or deliver drugs are broadly called medical wearables.
|
2017a
- (Izmailova et al., 2017) ⇒ Elena S. Izmailova, John A. Wagner, and Eric D. Perakslis (2017) . "Wearable Devices in Clinical Trials: Hype and Hypothesis". DOI: 10.1002/cpt.966. In: ASCPT - Clinical Pharmology & Therapeutics.
- QUOTE: For remote monitoring of cardiovascular parameters, activity (including gait, balance, and many other forms of motion measurement), body temperature, galvanic skin response, blood oxygen saturation, and multisensor/multisystem monitoring (Majumder et al., 2017), advanced wearable device research and development is continuously improving. Common form factors include wearable watches/bracelets, patches, textiles, and garments (Table 1). All of these sensor devices are being built with the ability to monitor continuously and communicate data in real time or intermittently. While maturity, promise, and quality all vary greatly at the moment, clearly these sensors and devices have the potential to become an integral part of the future of healthcare and biopharmaceutical development.
2017b
- (Majumder et al., 2017) ⇒ Sumit Majumder, Tapas Mondal, and M. Jamal Deen (2017). ["Wearable Sensors for Remote Health Monitoring"]. In: MDPI - Sensors 17(1), 130. DOI: 10.3390/s17010130.
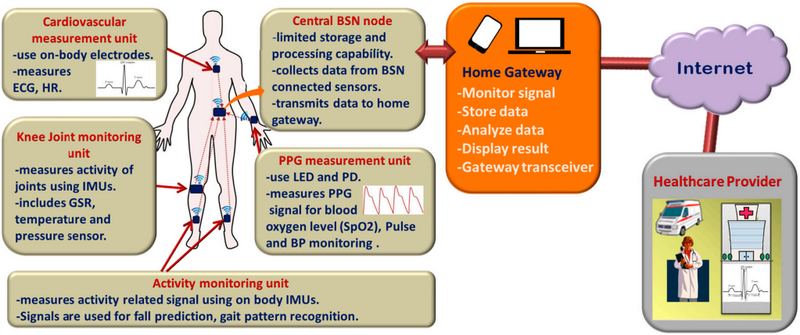
- QUOTE: The general overview of the remote health monitoring system is presented in Figure 1, although actual implemented system could differ depending on the application requirements. For example, some systems can be designed with few numbers of sensors where each of them can send data directly to the nearby gateway. In other systems, the sensors can be connected through a body sensor network (BSN) and the central BSN node gathers data from the sensors, performs limited processing before transmitting the data to the advanced processing platform.
|
2016
- (Steinhubl et al., 2016) ⇒ Steven R. Steinhubl, Evan D. Muse, and Eric J. Topo (2016). "The Emerging Field of Mobile Health". In: Science Translational Medicine, 7(283).
- QUOTE: These extraordinary advancements in mobile computer technology and connectivity have already transformed nearly every aspect of our lives: finance, travel, entertainment, education, and, of course, communications. However, only now are mobile health (mHealth) technologies making initial inroads into health care and, in so doing, are providing the foundation to radically transform the practice and reach of medical research and care. Through progressively miniaturized and increasingly powerful mobile computing capabilities, individuals are becoming increasingly capable of monitoring, tracking, and transmitting health metrics continuously and in real time. This metamorphosis has provided the potential for acute disease diagnosis and chronic condition management to take place outside the standard doctor’s office or hospital (Fig. 1).